Glaucoma FAQs
Glaucoma can strike people of any age, sex and race. However, the following factors may put you at increased risk:
- Being of African descent
- Having a family history of glaucoma
- Increasing age
- History of trauma to the eye
The risk of glaucoma increases markedly in people of African descent over age 35 and in people of Caucasian descent over age 50. Other risk factors for glaucoma include diabetes and possibly those with nearsightedness or high blood pressure.
What is glaucoma?
 Glaucoma is a disease of the optic nerve, which is the nerve that connects your eye to your brain. This nerve transmits visual information from the eye to the brain, allowing you to see.
Glaucoma is a disease of the optic nerve, which is the nerve that connects your eye to your brain. This nerve transmits visual information from the eye to the brain, allowing you to see.
Your vision can be impaired as optic nerve damage progresses and you begin to lose side vision.
In most cases, glaucoma damage progresses very slowly, over a period of several years. However, sometimes this damage can progress more rapidly. As the damage to the nerve progresses, a person begins to lose vision.
This loss of vision begins with the side, or peripheral, vision. You may be less aware of this part of your vision. Peripheral vision is very important in everyday activities such as walking and driving, keeping you from running into objects around you.
The loss of peripheral vision progresses as long as the disease is not treated. If treatment is not given, the visual loss can progress until it begins to involve the central, or reading, vision. At this point a victim of glaucoma may begin to notice vision trouble.
If treatment is still not given, then all vision in the eye can be lost. Visual loss from glaucoma is irreversible. Because vision lost from glaucoma can never be restored, it is critical to detect glaucoma before significant damage has occurred to the nerve. Proper treatment for glaucoma can be given to prevent further loss of vision.
What causes glaucoma?
High pressure inside the eye is known to cause glaucoma. The normal eye continuously produces and drains fluid internally in order to maintain the normal shape and pressure of the eye. This normal shape and pressure is necessary for you to see properly. In glaucoma, there may be a blockage of fluid drainage or an excess of fluid production, which leads to high pressure inside the eye. If you have high eye pressure, the increased pressure may damage your optic nerve. Some people, however, are able to tolerate high eye pressure without developing glaucoma damage to the optic nerve. The reason for this is unknown. The Ocular Hypertension Treatment Study has shown that treatment of increased eye pressure reduces the risk of developing glaucoma by half for some people.
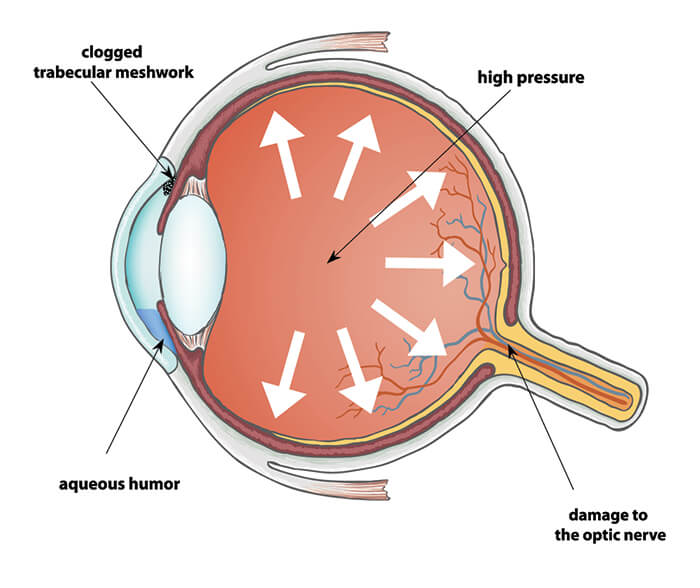
Pressure Building in the Eye
Some people develop glaucoma even without evidence of increased pressure inside the eye. In fact, recent studies show that up to 50% of people with glaucoma may not have high eye pressure measurements. For example, persons of Japanese descent are more prone to have glaucoma without elevated eye pressure, and “normal pressure” glaucoma is more common in Japan than “high pressure” glaucoma.
Many studies are in progress to discover the reason for glaucoma damage in people who do not have increased eye pressure. The two leading theories are that damage to the nerve is caused by poor circulation to the nerve, or that abnormally high concentrations of naturally occurring chemicals or hormones cause the damage.
Scientists who believe that poor circulation causes glaucoma have used special ultrasound testing to show decreased blood flow to the eyes of some people with glaucoma. Many of these people with “normal pressure” glaucoma also have other problems with their circulation, such as heart disease, poor circulation to their legs and feet, or hardening of the arteries.
Other scientists have shown increased concentrations of glutamate and other chemicals in the eyes of people with glaucoma. These chemicals are naturally produced by the body, and in normal amounts, help with normal eye functions. In abnormally high concentration, however, these naturally-occurring chemicals can actually harm the very nerve tissues from which they are produced. The scientists still have not discovered why the body produces abnormally high amounts of these chemicals in eyes with glaucoma.
Doctors and scientists are working to discover treatments for poor circulation to the optic nerve and treatments to decrease the concentration of these harmful hormones in the eye. Studies are under way to determine if improving circulation or decreasing the hormone concentration will help stop damage from glaucoma.
How is glaucoma diagnosed?
A normal healthy nerve has a small cup-shaped hole in the center.
When your eye doctor examines your eye, he or she can detect glaucoma damage by the appearance of your optic nerve. A normal healthy nerve has a small cup-shaped hole in the center (see photo). As damage from glaucoma progresses, this hole in the center of the nerve enlarges and replaces the healthy nerve tissue.
Your eye doctor can detect progression of the disease by periodically examining the appearance of the nerve. Your doctor also may photograph the nerve to document the appearance at a specific point in time. This allows better comparison in the future to be certain the disease has been stabilized. These photographs, called disc photos, are particularly helpful if your doctor has decided that you are a “glaucoma suspect.”
As damage from glaucoma progresses, this hole in the center of the nerve enlarges, and replaces the healthy tissue of the nerve.
A glaucoma suspect is a person whose optic nerve appearance is suspicious for glaucoma, but does not demonstrate definite glaucoma damage. If you are a glaucoma suspect, your doctor will want to examine your optic nerve two or three times a year and compare to the baseline disc photos to detect definite glaucoma damage as soon as it occurs.
This early detection will allow your doctor to begin treatment before the glaucoma has a significant effect on your vision. A relatively new method of evaluating early glaucoma damage to the optic nerve is Heidelberg Retinal Topography (HRT). HRT uses a laser to scan the surface of the nerve, and then a computer determines if there has been any change from previous examinations.
Another way to measure the amount of nerve damage is to measure the amount of peripheral or side vision that has been lost. Glaucoma does not affect your central reading vision until the late stages of the disease. At this late stage, a glaucoma victim may already be partially blind. Therefore, it is important to measure the peripheral vision in the early stages of the disease, so that proper treatment can be given to prevent blindness. This is accomplished with visual field testing, which is an examination that measures the amount of vision lost.
To test the visual field, your doctor uses an instrument that flashes lights of various intensities. You place your head against a head rest and stare at a target light directly in front of the eye being tested. The machine then flashes lights in your peripheral (side) vision. Some of these lights are bright and easy to see. Others are so dim that they are impossible to see even if you have no visual damage. Most lights are somewhere in between.
When you see the light, you press a button and the machine registers your response. The machine then prints out a map showing any areas that you cannot see properly. Your eye doctor can repeat this measurement periodically to determine if the glaucoma treatment has been effective in stabilizing the damage.
There are other types of specialized testing that have recently become available, such as measurement of the thickness of the nerve with a technique called scanning laser polarimetry (GDx Nerve Fiber Analyzer) or optical coherence tomography (OCT) and short wavelength perimetry, which uses colored lights to test the visual field (peripheral vision). Both of these technologies are particularly helpful if a person is suspected of having glaucoma, but there is no definite damage visible (glaucoma suspect).
Are there different types of glaucoma?
The most common type of glaucoma is open angle glaucoma. Open angle glaucoma means that there is no visible obstruction to the drainage area inside the eye. It is thought that there may be an invisible obstruction to fluid drainage in the trabecular meshwork, which is the structure in the eye that drains the fluid.
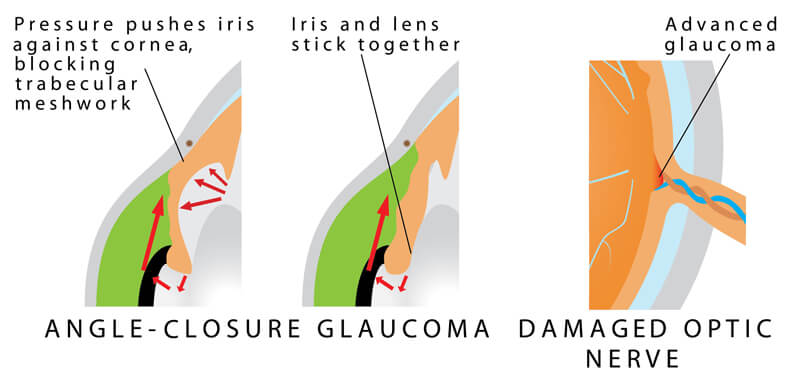
Another type of glaucoma is narrow angle glaucoma. In this condition, the iris of the eye causes an obstruction to the drainage area inside the eye.
This type of glaucoma is most common in persons of Chinese descent and Vietnamese descent, and less common in persons of African and Caucasian descent. However, it can affect a person of any race. This type of glaucoma may cause symptoms of sudden pain, redness, blurred vision, and colored haloes around lights. This condition is called acute narrow angle glaucoma and must be treated immediately.
Failure to treat this condition immediately can cause permanent loss of vision. Sometimes narrow angle glaucoma is a chronic condition that does not cause any symptoms, like open angle glaucoma. Your doctor can determine if you are at risk of narrow angle glaucoma by performing a procedure called gonioscopy.
How is open angle glaucoma treated?
There are several ways to treat open angle glaucoma.
Eye drops and medication
Most commonly, treatment begins with eye drops that are designed to lower the pressure in the eye. These drops are used from one to four times daily, depending on the medication. These drops are designed to decrease the amount of fluid produced in the eye, or to increase the amount of fluid drained from the eye.
Oral medications also are available to lower the eye pressure. Like all medications, these eye drops can have side effects. When treatment with eye drops is started, you should discuss with your doctor the potential side effects and interactions with other medications that you may be taking.
Laser treatment
Another way of treating glaucoma is with a laser. This laser is designed to increase the amount of fluid drained from the eye, thereby lowering the pressure in the eye. The laser treatment is usually performed in the office, takes only a few minutes, and is normally painless.
Microsurgery
The third way to treat glaucoma is with microsurgery in the eye operating room. In this procedure, a small drainage hole is created in the eye, usually behind the upper eyelid. This allows fluid to drain out of the eye and into the circulation behind the eye in the eye socket. This drainage allows the eye pressure to be lowered, thereby preventing further damage from glaucoma.
Open angle glaucoma is generally a disease that stays with an affected person for life. Whether the treatment has been with medications, laser or microsurgery, the victim of glaucoma must continue to be monitored by the eye doctor several times a year.
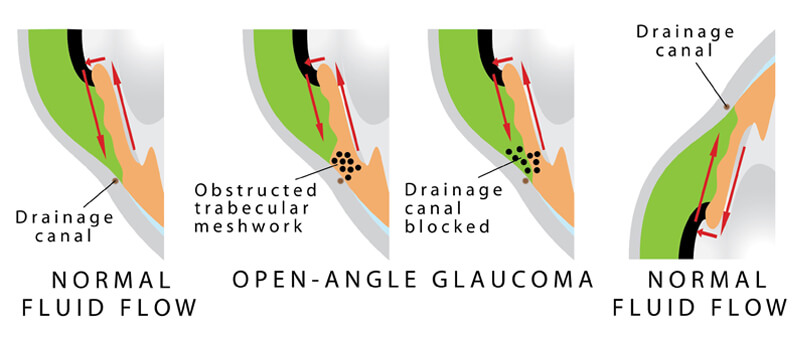
Diagram of Open Angle Glaucoma
Your doctor will monitor the eye pressure, the appearance of your optic nerve. The doctor also will periodically test your peripheral, or side, vision (visual field) to be certain that the disease has been stabilized, and that further vision loss will not occur.
How is narrow angle glaucoma treated?
Your eye doctor will check to see if you have a narrow drainage area in your eye in order to know if you are at risk of developing narrow angle glaucoma.
Your doctor will perform an examination known as gonioscopy to evaluate your risk. If you are at risk for narrow angle glaucoma, your eye doctor will recommend a preventive laser treatment. If you already have narrow angle glaucoma, sometimes it can be cured with the laser treatment.
Sometimes narrow angle glaucoma is a chronic condition that is treated with the same medicines or microsurgery described above for open angle glaucoma.
How can I be sure that glaucoma does not affect my vision?
The best way to prevent visual loss from glaucoma is through regular eye examinations by an eye doctor. Your eye doctor will help you to determine the most appropriate follow-up schedule for you.
More frequent examinations (every 1-2 years) are recommended if you have any problems with your vision or have a family history of glaucoma. More frequent examinations are also recommended if you have certain medical conditions, such as diabetes or high blood pressure.
For children, routine annual screening examinations by the pediatrician are usually sufficient, unless an eye appears abnormal or if the child has trouble seeing.









