Visual field (VF) testing is a common tool practitioners use in monitoring progression and staging glaucoma in our patients. The gold standard in glaucoma visual field testing has always been Humphrey Visual Field (HVF) 24-2. This test allows us to monitor the central 24 degrees of field, totalling 54 points that are 6 degrees apart (1). In glaucoma, it is important to monitor for glaucomatous VF defects in these peripheral and central points, and use changes in VF defects to influence changes in treatment. Most commonly, we are looking to identify nasal step, partial arcuate, arcuate, and paracentral VF defects correlating with optic nerve changes. What is often overlooked in VF testing, for all stages of glaucoma, is the importance of 10-2 central VF testing.
Central 10-2 VF testing should be considered in all stages of glaucoma, including early glaucoma. It is easier to consider the importance of central VF testing in patients with severe glaucoma, with apparent central field changes. What is less apparent, is recognizing the benefit of central VF testing in the management of patients with early or mild glaucoma. If a mild glaucoma or glaucoma suspect patient has central field changes upon 24-2 testing, it is important to run baseline 10-2 testing, in order to provide for proper baseline and prevent mis-diagnosis of staging (2). One may even consider running a baseline 10-2 field test on all glaucoma patients in order to provide baseline to compare future changes. Early glaucoma patients may show changes to the ganglion cell complex prior to the retinal nerve fiber layer on OCT testing, thus having early central field involvement. These manifestations will lead to macular field changes prior to peripheral field changes upon VF testing (6). This is especially true in patients with normal presenting pressure, which tend to progress earlier on ganglion cell layer testing than retinal nerve fiber testing; presenting first with paracentral VF defects (7). In patients with early glaucoma, up to 60% of patients who test normal on 24-2 testing were considered abnormal upon 10-2 visual field testing (2). These central defects in early glaucoma patients are more commonly seen in the upper VF and may have an arcuate pattern closer to fixation than those in the inferior VF (3,7). Additionally, early glaucoma patients with central defects upon baseline 24-2 testing are associated with increased rate of global progression. Thus, identifying central defects early in the disease process and following these patients with 10-2 VF testing, aids in identifying high-risk patients who may need a more intensive management regimen (5).
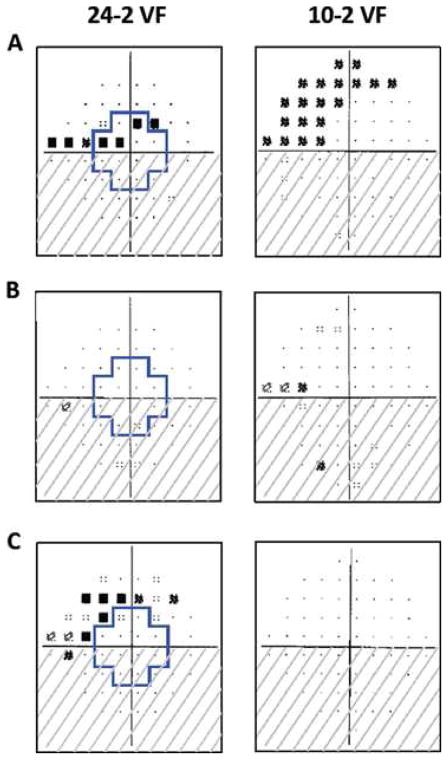
Figure 1:
The region within the blue cross on the 24-2 VFs corresponds to the region in the central 10° tested by the 10-2 VF test points. A) Both fields show superior hemifield defects. B) Superior hemifield defect is seen on 10-2, but missed on 24-2 testing. C) Superior hemifield shows central defects on 24-2, however is normal on 10-2. (4).
In patients with extensive peripheral VF changes, and/or paracentral and central defects, it is also important to recognize the limitations 24-2 VF testing has for glaucoma diagnosis and management. With severe stages of glaucoma, the peripheral VF points on 24-2 testing are more likely to be significantly reduced in sensitivity and may produce absolute defects. Because of this, these peripheral points are less likely to show significant changes in sensitivity, thus masking smaller changes occuring in the central VF points. A point of mention while using these modes of testing in glaucoma, is to be aware of mean deviation (MD) changes. Mean deviation is an index on visual field testing, which allows us to quantify the severity of VF loss. Especially in severe stages of glaucoma, the rate of change seen in 10-2 visual fields is significantly greater than that of 24-2 VFs (1). Additionally, 24-2 VF testing only utilizes 12 of its total 54 testing points for central vision. Of these 12 points tested, only 4 are actually in the central 8 degrees of the macular field (3). By incorporating 10-2 VF testing, we are able to specifically focus our testing to the central 10 degrees of our visual field. This central field is tested in high detail with 68 points that are 2 degrees apart. (1) Thus, when only using 24-2 visual field testing for these types of patients, true glaucomatous progression may be erroneously missed. This emphasizes the importance of using central 10 degree testing to monitor for changes or progression in our advanced stages of glaucoma.
References:
- Rao, H.L. et al. “Comparing Glaucoma Progression on 24-2 and 10-2 Visual Field Examinations”PLoS One. 2015; 10(5): e0127233.
- De Moraes, C. Gustavo et al. “24-2 Visual Fields Miss Central Defects Shown on 10-2 Tests in Glaucoma Suspects, Ocular Hypertensives, and Early Glaucoma” Ophthalmology, Volume 124, Issue 10, 1449-1456.
- Lifferth, Austin et. al. “10-2 Visual Field Testing: A Tool for All Glaucoma Stages” Review of Optometry. Jul 15, 2017.
- Traynis I et al. “Prevalence and nature of early glaucomatous defects in the central 10° of the visual field.” JAMA Ophthalmol. 2014 Mar;132(3):291-7.
- Garg, Aakriti et al. “Baseline 24-2 Central Visual Field Damage Is Predictive of Global Progressive Field Loss” American Journal of Ophthalmology, Volume 187, 92-98.
- Hood DC et al. “Early glaucoma involves both deep local, and shallow widespread, retinal nerve fiber damage of the macular region.” Invest Ophthalmol Vis Sci. 2014 Feb 3;55(2):632-49. doi: 10.1167/iovs.13-13130.
- Marshall, H.N. et. al. “Macular Ganglion Cell-Inner Plexiform Layer Loss Precedes Peripapillary Retinal Nerve Fiber Layer Loss in Glaucoma with Lower Intraocular Pressure.” American Academy of Ophthalmology 2019; 126:1119-1130.

Author: Emily Bucher, OD, FAAO
Seattle Clinic
Since September, I have been working alongside our glaucoma specialist in Seattle, Dr. Bruce Cameron. Joining the team with Drs. Cameron, Jones, and Clermont, is an exciting new collaboration at NWES which allows us to manage many more glaucoma patients at the clinic. Being able to work closely with referring doctors, in the management of their glaucoma patients, has been an enjoyable addition to my work at NWES. While increasing my glaucoma patient base, the emphasis and importance of proper visual field testing in glaucoma management has been a crucial part of many patient exams. This post is an important reminder of the many benefits 10-2 VF testing can provide in our management of glaucoma.









